We’re Not Just Tired
February 5, 2020
In the morning, after the grogginess of 7 am has worn off, after first period finishes, wakefulness sets in. Students get chattier and more ready to take on the day, but for some students the grogginess never wears off and they don’t get to feel awake.
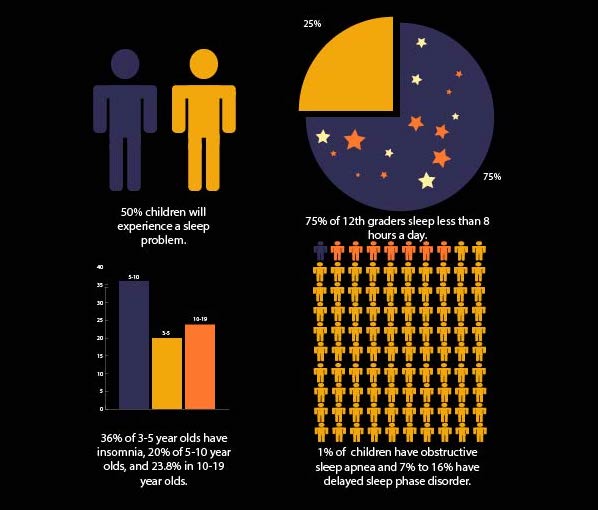
According to the American Academy of Family Physicians, up to 50% of all children will at some time experience a sleep problem. Whether that problem is short term or evidence to suggest a sleeping disorder can be a fine line that is difficult to differentiate. There are multiple sleep disorders that can go unnoticed in children and teens. Sleep apnea, insomnia, sleepwalking, and narcolepsy can have detrimental effects on teens if the signs are overlooked or dismissed. The American Academy of Sleep Medicine stated that “insufficient sleep among adolescents may not only contribute to lower grades and a lack of motivation, but may also increase the odds of serious levels of emotional and behavioral disturbances.” With sleep as a cornerstone to success for people of all ages, especially students, it is important to recognize when an issue is present.
Disturbances in sleep resulting in an individual being unable to fall asleep or stay asleep is called insomnia, per the Cleveland Clinic, and can have detrimental impacts on a student’s life both in the short term and long term. It can be traced back to things such as stressors in their life, caffeine, a side effect of medication, depression, anxiety, medical problems, pain, or environmental factors like the amount of light in the room or temperature. If insomnia is consistent it can lead to tension, irritability and mood swings, depression, aggression, memory issues, among a handful of other things.
Megan O’Brien ’21 is very familiar with insomnia and the trouble in recognizing the issue. “I’ve probably had insomnia since seventh grade and it was one of those things, I had always stayed up late reading but it kind of became a problem when it wasn’t a choice to stay up, I couldn’t sleep,” O’Brien said. “I’ve only been diagnosed with insomnia for about a year now. I realized that it was a problem in eighth or ninth grade but I really didn’t take steps to do anything about it until last year because it seemed more normal to me, I just figured it was something everybody dealt with.”
The impact insomnia had on her life was large and not easy to overcome. “There have been times when I literally haven’t slept for 48 hours and I’m falling asleep in classes, and I don’t have the energy to go out or to do things,” O’Brien said. “I mean my grades definitely took a hit from that because I was exhausted all the time. But when I was trying to go to sleep I couldn’t.”
Prior to diagnosis, O’Brien was searching for a remedy to help her fall asleep. “I tried over the counter drugs like melatonin before I ended up being medicated and it was one of those things like it would work for a couple of days and then that’s it because my body would build up a tolerance,” O’Brien said. “My body really didn’t want to sleep. It’s maddening, even still. Even medicated, I take drugs every single night to put me to sleep, it can still take me a couple hours to get to sleep and that’s good for me. I feel like I’m going crazy, in a way, because I just don’t get how people can just lay down in bed and go to sleep.”
Just as the Cleveland Clinic noted can occur, her insomnia is worsened by mental health disorders. “I have anxiety and depression as well so when I was diagnosed with insomnia it was kind of a joint diagnosis because things like anxiety and depression can lead to insomnia,” O’Brien said. “I have a chemical imbalance, that’s why I’m an insomniac just in general but because I have anxiety and depression it makes it ten times worse than it already would have been.”
But overall, since the diagnosis O’Brien has been able to cope with her insomnia and fight it. “It’s always a process because you kind of have to tinker around with medications to get the right dose but I have definitely slept better,” O’Brien said. “I’ve had better and deeper sleep. I’ve been able to sleep faster, my grades have definitely improved, I’ve felt more alert, and I felt that I could interact with people better, and that I could go out and do things with friends without feeling like I had just run a marathon.”
The Mayo Clinic describes pediatric sleep apnea as “a sleep disorder in which your child’s breathing is partially or completely blocked repeatedly during sleep…due to narrowing or blockage of the upper airway during sleep.” It is a common and typically chronic disorder that can be potentially dangerous and occurs in 1-5% of children according to the American Association of Family Physicians. If left untreated long-term it can prevent growth and cause heart problems. In the short term, those with sleep apnea feel tired even when sleeping the whole night, often snore loudly, have difficulty paying attention, and may have learning or behavioral problems.
Per the National Institute of Neurological Disorders and Stroke narcolepsy is a rare, chronic sleep disorder of the brain that causes the individual to experience excessive daytime sleepiness. A narcoleptic could also experience sleep attacks, cataplexy, hallucinations, sleep paralysis, fragmented sleep, and in some cases insomnia. It is caused by a lack of a chemical in the brain responsible for regulating wakefulness as well as going in and out of REM sleep. This causes narcoleptics to spend too much time in REM sleep when dreams occur resulting in sleepiness.
For two years, I woke up after 10+ hours of sleep feeling more tired than the night before, not knowing that I was fighting narcolepsy. Countless naps and cups of coffee could not combat the overwhelming exhaustion that relentlessly plagued me day in and day out. Constantly listening to music gave me just enough to focus on so that my eyes stayed open in class but the need to slump over onto the desk never subsided. Some days were better than others but the story was the same: no matter how desperate I was to feel awake exhaustion was my closest friend and didn’t leave my side. Going to school became a constant war with trying to keep myself awake in class as the daily battle I did not always win. Completing my homework each night meant having to convince myself that doing it would be more worth it than closing my eyes and feeling relief.
How I was feeling went unacknowledged for a while, then it was swept under the rug as being a temporary thing. Regardless of how much I emphasized how tired I was it was underestimated and it continued to take its toll on my life. My grades, my friendships, my relationships with my family all struggled and no one could explain why.
Payton Blahut ’21 has been diagnosed with both sleep apnea and narcolepsy, a combination that is rarely seen. “Sleep apnea and narcolepsy are almost polar opposite so it’s weird to have them together,” Blahut said. “With narcolepsy I can fall asleep in an instant but with apnea I’m awake every minute.”
She remembers the symptoms and the impact they had on her life at an early age. “I think it was second grade,” Blahut said. “I remember being really really upset when my mom would wake me up in the morning. Like any kid I would fight going to school but my mom tells me now that it was more than just that, she could tell there was something up. The second that she would give in, I would just fall back to sleep right away, and even if she would make me go to school I would fall asleep in school.”
Sleep apnea, however, was a different battle. “Sleep apnea is when you stop breathing in the middle of the night and I stop breathing 40 to 50 times per hour,” Blahut said. “So my throat bleeds in the middle of the night sometimes which is not fun.”
Before someone can be diagnosed with narcolepsy, they have to be tested for sleep apnea. In her case, testing positive delayed diagnosis of narcolepsy for months. “You do the night test first and then you do the morning test,” Blahut said. “If you test positive for sleep apnea, they cancel your morning test so I had to fight to stay in that morning test. I have a pretty high amount of sleep apnea. So they do that portion and she woke me up at 6 am and said ‘yeah there was a bit of sleep apnea on your registry, so we’re going to send it to the doctor and if he thinks it’s enough we’ll do your narcolepsy test’. So they cancelled it.”
Blahut’s doctors won’t medicate her for narcolepsy meaning the symptoms of it, namely excessive daytime sleepiness, continue to affect her day to day. “Last year I had over 300 absences, that’s periods,” Blahut said. “I could obviously be doing better in my classes if I was there and I’ve been threatened with getting dropped from classes if I wasn’t there for seat time. The thing I’ve heard from my counselor is if you miss 20 periods of a class in one semester you’re automatically dropped, failed, even if you have an A.” The school has tried to help, but her options are limited and coping can be a difficult battle. “They talked about giving my first hour free, but that’s it and they haven’t. What I’ll do is I’ll show up for those first three periods of the day and then I’ll just go home. Even my mom was getting upset at that point.”
Sleep apnea, insomnia, and narcolepsy are devastating disorders to try and manage if they go unacknowledged for a long period of time. Their symptoms and effects on one’s life, particularly teenagers, can negatively impact grades, relationships, and mental health. “Before I knew what was going on I felt like there was something wrong with me,” Blahut said. “Especially when I was put on depression medication and none of that was working. I was like ‘why isn’t this working, there has to be something wrong with me, maybe I’m a weird, freak case, what’s happening’. I could not lift myself out of bed most days.”